What causes PCOS ? Some new ideas on an ancient disease and modern women

Sometimes I am asked – is PCOS caused by eating too much sugar, unhealthy fat and our sedentary lifestyle? Interestingly, the disease of PCOS does not appear to increase in areas of the world where obesity is more prevalent. This indicates that this disease is not caused primarily by obesity. There are many ancient medical records describing women with PCOS conditions (including prolonged menstrual cycles, infertility, acne, abdominal fat, and hirsutism). A recent article in Fertility and Sterility proposes that PCOS is actually an ancient genetic condition that has persisted over thousands of years in women. But why would PCOS persist in our gene pool when it leads to infertility or decreased reproduction in women?
Ancient Hunter-Gatherer communities and women with PCOS
There are several reasons why PCOS variants may have persisted in women over thousands of years. In ancient hunter gatherer communities those who had metabolisms which conserved energy and stored fat had definite survival benefits. Women with PCOS do carry these metabolic advantages. They tend to be metabolic energy conservers – something which is of great advantage in times of low food supply. Because women with PCOS generally had fewer children due to reduced fertility rates, they often had the survival advantage of caring for only one young child at a time and had greater resources for themselves and their families. Childbirth related complications were a common cause of death, so women with pcos were also at a survival advantage due to decreased maternal mortality. In ancient cultures, there was less food supply, more physical activity and therefore less obesity, so women with PCOS generally had a lower BMI (Body Mass Index) compared to modern women. At times when food was in short supply, women with PCOS would tend to have more normal BMIs (leading to more normal levels of fertility). At these same times, women without PCOS would have lower BMIs and may have been more prone to have subfertility themselves.
Generally, fertility is lower amongst women with PCOS at all BMI levels. In times when BMIs are on average lower in the population, women with PCOS will have more normal reproductive rates. . This illustrates the importance of achieving a healthy BMI for women with PCOS and that the condition actually is one of subfertility rather than infertility.
Please view the following table to see the relationship of BMI to fertility in women with and without PCOS variants:
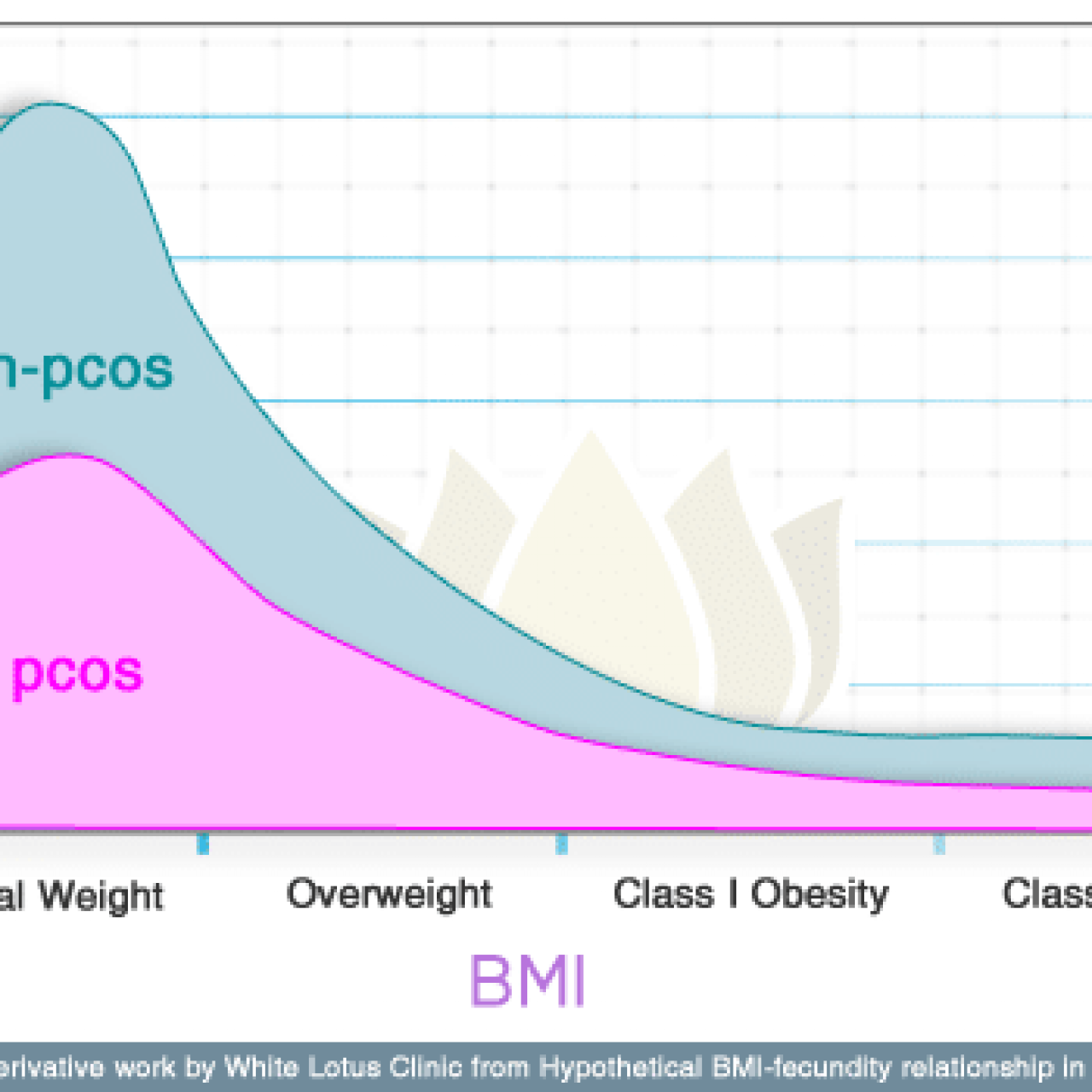
Figure 1: Hypothetical BMI-fecundity relationship in PCOS. © 2010 American Society for Reproductive Medicine
Another point to consider is that PCOS genes are also carried through males, who also carry these metabolic survival advantages and do not experience subfertility. PCOS genetic variants include greater lean muscle mass and bone density and these males could pass on these beneficial genes to their offspring. This explains how this genetic type could persist through thousands of years even though it is related to subfertility.
How This Translates to Modern Women
In general, BMI levels tend to be increased with the modern western diet and lifestyle, so the effects on reproduction of PCOS are amplified compared to those in ancient times. Women with this condition must pay extra attention to achieving a healthy BMI. Although having a high BMI does not cause PCOS, it will definitely cause lower fertility levels. For those women who have a high level of insulin resistance (which is aggravated by the western diet), extra attention must be paid to working with insulin balance in the body. This can be done very effectively with the right diet and supplements.
Integrative Medicine Assessments
PCOS variants should be screened for in all women seeking fertility treatment who have a long cycle, acne, hirsutism, or abdominal fat accumulation (even in slimmer women). Many traditional assessments can miss mild cases of this condition or “leanings” towards the condition. Restoring pituitary and metabolic function in these women can effectively restore fertility and often heavy medical intervention is not required.
- The Following Tests Should be Completed
- Glucose to insulin ration and oral glucose tolerance testing
- HBA1C
- Day 3 LH to FSH ratio
- Full early AM androgen panel – (androstenedione, free testosterone, DHEA-S, 17-OH Progesterone)
- AM cortisol or diurnal cortisol
- Transvaginal pelvic ultrasound to check for cystic ovaries
In a women who has an elevated LH to FSH ratio we can assume much of the PCOS is related to hypothalamic pituitary dysfunctions. With a normal LH to FSH ratio other metabolic disorders are often more prevalent and contributing factors should be identified. Androgen balance is of great importance, and elevated levels should be identified. It is also important to note that PCOS variants can be closely mimicked or aggravated by adrenal conditions so assessment of the adrenal function including diurnal cortisol, and DHEA-S testing is very important. It is also important to rule out other causes for lack of/delayed ovulation such as elevated prolactin levels or clinical/subclinical thyroid disease.
PCOS Treatment
PCOS Treatment very much depends on the individual characteristics of each woman’s condition. There are many different PCOS variants as this is a syndrome involving reduced frequency of ovulation and is not a discrete disease with one cause. A patient does not have to have all of the diagnostic criteria of PCOS to have her fertility affected by a milder variant of this disease. Each patient will require different treatment based on her lab values, metabolic characteristics, body type, severity of disease and level of inflammation. We take all of this into account, for instance when treating PCOS naturally through our Toronto Naturopathic Clinic.
Hunter-Gatherer Diets and PCOS
Returning the patient to a healthy bmi is much more important for fertility than in women without PCOS. Thus, healthy diets with attention to glycemic index are of great effectiveness. I always counsel patients with PCOS extensively on nutrition and diet as this is an area of special need for them even if they are a “lean” type. A hunter-gatherer diet is often the best type of diet for pcos. This diet is high in healthy proteins such as lean meats, seafood, fruits and berries, vegetables, and nuts and low in grains. Most especially of course, the diet should be low in sugar since hunter gatherer cultures had very low sugar intake overall.
A simple one day hunter-gatherer diet for PCOS variants:
- Breakfast: Omelette made with onions and spinach.
- Snack: Ambrosia (pear, avocado and 1/2 unripe banana – blend in blender until smooth and creamy) *Did you know unripe bananas have a glycemic index of 50 whereas a ripe banana has a glycemic index of 82
- Lunch: Tilapia fillet drizzled with olive oil, with brocolli or salad (dressing of fresh lemon, olive oil and fresh herbs)
- Snack: sliced baby cucumber with fresh lemon squeezed on top. 3 tbsp almonds and 1 cup of fresh blueberries
- Dinner: Grilled chicken breast with pesto and baby bok choy
This diet would be varied with respect to quantity and calories for differing weight loss or maintenance requirements.
Supplements
I use supplement therapy as a mainstay along with diet in the treatment of PCOS and have found the combination works wonderfully to restore cycle regularity. Supplements are aimed at restoring normal hypothalamic-pituitary function, increasing antioxidant status, improving insulin resistance, and minimizing excess androgen levels if required. Supplement protocols will vary widely with different “types” and lab results found in different pcos variants.
References
- Carmina E, Guastella E, Longo RA, Rini GB, Lobo RA. Correlates of increased lean muscle mass in women with polycystic ovary syndrome. Eur J Endocrinol 2009;161:583–9.
- Di Carlo C, Shoham Z, MacDougall J, Patel A, Hall ML, Jacobs HS. Polycystic ovaries as a relative protective factor for bone mineral loss in young women with amenorrhea. Fertil Steril 1992;57: 314–9.
- Good C, Tulchinsky M, Mauger D, Demers LM, Legro RS. Bone mineral density and body composition in lean women with polycystic ovary syndrome. Fertil Steril 1999;72:21–5.
- Ricardo Azziz, Daniel A. Dumesic, Mark O. Goodarzi. Polycystic ovary syndrome: an ancient disorder? Fertility and Sterility – 27 October 2010
- To WW, Wong MW. A comparison of bone mineral density in oligomenorrhoeic adolescents with polycystic ovaries and normal ovaries. Gynecol Endocrinol 2005;20:237–42.